F- CLINICAL ASPECTS OF SPINAL CORD INJURIES
535
Passive movements of all joints of the paralysed limbs should be carried out at least
three times daily and, if possible, more often in the acute stage of paraplegia to promote
better circulation in the paralysed limbs and prevent oedema and contractures. However,
flexion and abduction movements should be carried out gently and with care. Maximal
abduction and flexion of the hip over 90° should be avoided in the stage of flaccidity
during the spinal shock period, as brisk and too extensive passive movements may lead
to haemorrhages in the tissues around the hip joints which may facilitate the formation
of para-articular ossification. Moreover, there is also the danger of producing fractures or
dislocation of the femur in cases with lower motor neurone lesions resulting in atrophy
and osteoporosis. In incomplete cord and cauda equina lesions, auto-assisted movements
should be started within the first few days after injury, and the patient should be encour
aged to improve the function of partly paralysed muscles himself as often as possible
during the day, after having been instructed about the technique by the physiotherapist.
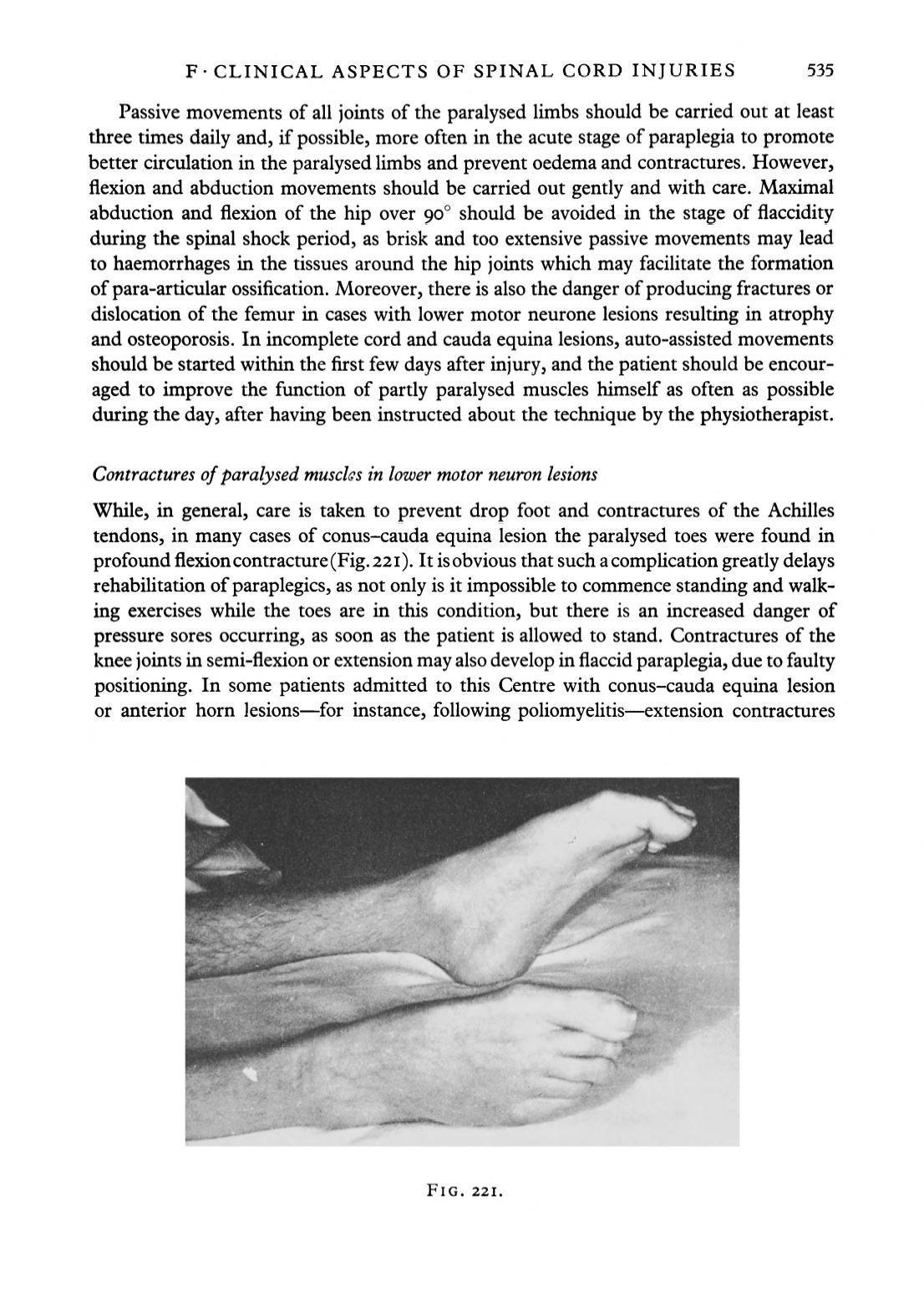
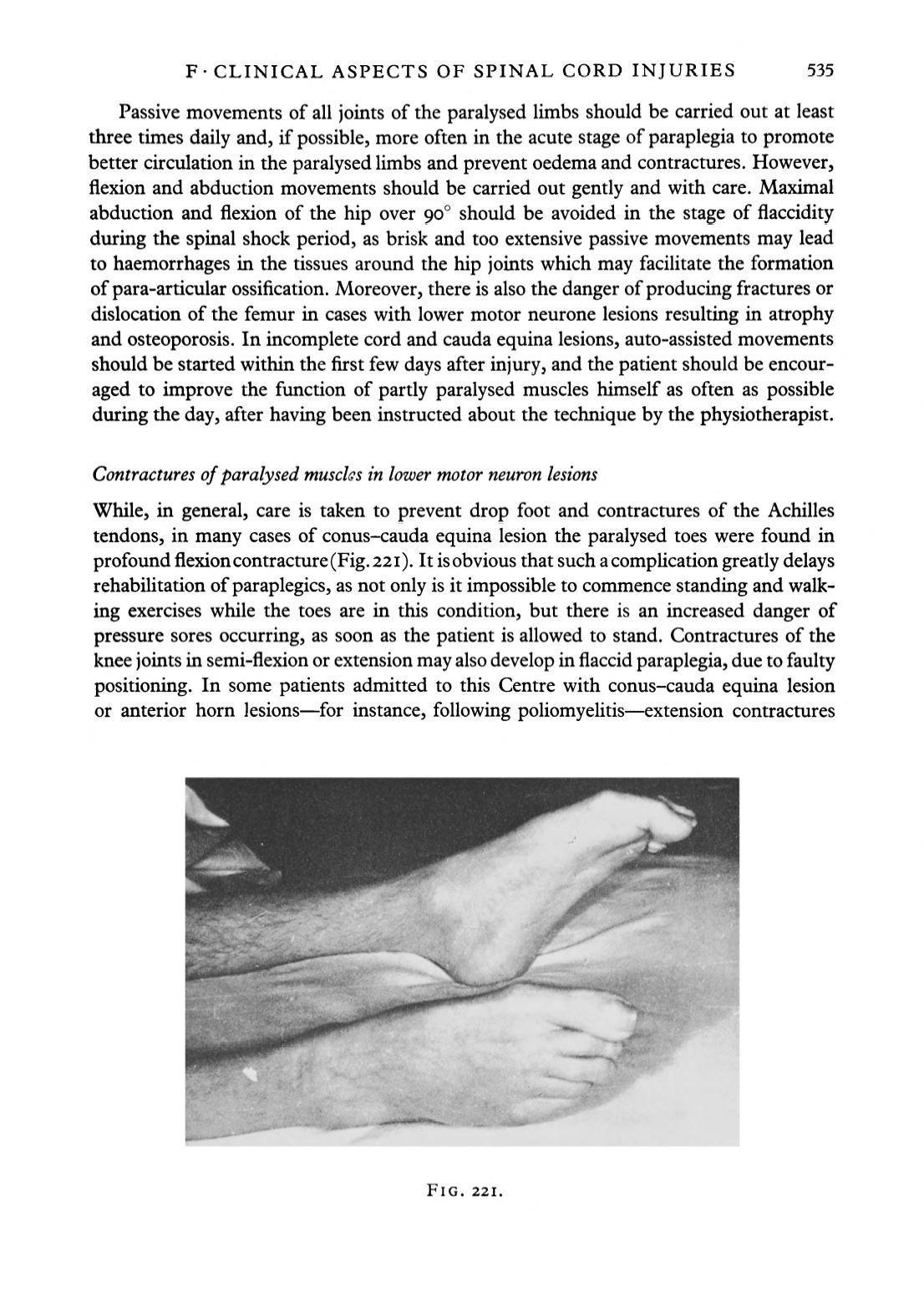
Contractures of paralysed muscles in lower motor neuron lesions
While, in general, care is taken to prevent drop foot and contractures of the Achilles
tendons, in many cases of conus-cauda equina lesion the paralysed toes were found in
profound flexioncontracture (Fig. 221). It is obvious that such a complication greatly delays
rehabilitation of paraplegics, as not only is it impossible to commence standing and walk
ing exercises while the toes are in this condition, but there is an increased danger of
pressure sores occurring, as soon as the patient is allowed to stand. Contractures of the
knee joints in semi-flexion or extension may also develop in flaccid paraplegia, due to faulty
positioning. In some patients admitted to this Centre with conus-cauda equina lesion
or anterior horn lesions—for instance, following poliomyelitis—extension contractures
FIG. 221.